Cervical osteochondrosis is a lesion of the vertebral discs of the cervical spine, as a result of which they undergo degenerative-dystrophic changes. The main reason for its development is a violation of the normal course of metabolic processes, which leads to a distortion of the structure of the vertebral bodies and cartilaginous discs. In the case of localization in the neck, the symptoms of pathology are largely determined by the compression of large vessels. Treatment methods are selected depending on the stage, the specificity of the course, the severity, the main symptoms.
Features of the disease
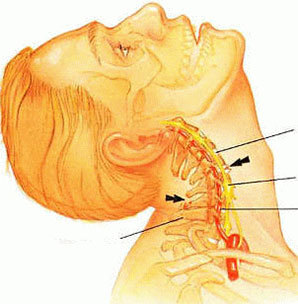
The cervical form is the most dangerous type of osteochondrosis: it leads to a deterioration in cerebral circulation, since the vertebral artery passes through this area - one of the largest vessels supplying the brain with the necessary substances and oxygen.
Displacement of the vertebrae, abnormal changes and overgrowth of bone and fibrous tissue disrupt the normal functioning of the vessel.
The specificity of the symptoms of osteochondrosis in this part is determined, among other things, by one of the structural features of the cervical vertebrae, which consists in their closer adherence to one another. As a result, any change in one segment provokes the failure of the entire department.
Clinic depending on the stage
In the process of its development, cervical osteochondrosis goes through four stages. How does it manifest itself on each of them?
- Stage 1. It is characterized by the appearance of initial disturbances in the stability of the intervertebral discs. Symptoms are mild or absent. Not very pronounced pain sensations and local muscle tension are possible.
- Stage 2. The disc protrusion begins, the gaps between the vertebrae are reduced, the annulus fibrosus collapses. In many cases, as a result of compression of the nerve endings, pain appears - mainly of a point nature. They intensify when turning, tilting the neck. Decreases tone, weakness often appears.
- Stage 3. The process of final destruction of the fibrous ring leads to the formation of hernias. This stage is characterized by a significant deformation of the spine. Increased pain and fatigue occur against the background of sensory disorders and limited mobility in the affected area.
- Stage 4 is the most difficult. Intense pain syndrome manifests itself with any attempts to move, which entails a significant limitation of the mobility of this department. At times, the pain subsides, but this does not show an improvement in the condition, but only indicates an increase in the size of bone growths, which significantly limit movement. They often lead to patient disability.

Symptoms of cervical osteochondrosis
When located in the cervical spine, the prevailing symptoms of osteochondrosis are:
- pain in the neck, back of the head, shoulder, arms;
- restriction of movements, crunching at various turns, neck tilt;
- weakness in the hands;
- pulling pain in the left side of the chest, radiating to the corresponding arm;
- burning in the interscapular zone;
- recurrent headaches;
- weakness;
- dizziness (with severe course of cervical osteochondrosis, it can reach loss of consciousness);
- coordination of movements is impaired, which is mainly reflected in gait;
- hearing impairment, ringing in the ears;
- decreased vision;
- sore throat;
- poor dental health;
- weakening or hoarseness of the voice;
- snoring is a consequence of the tension in the neck muscles.
In the cervicothoracic type, the symptoms are almost similar to those of cervical osteochondrosis. This:
- asthenic syndrome;
- dizziness and headaches;
- periodic pressure fluctuations;
- flashing flies before the eyes;
- pain in the shoulder girdle and arms;
- muscle weakness;
- numbness, tingling, chilliness of the fingers;
- pain in the chest, heart area;
- nausea;
- numbness of the tongue, face;
- dental problems;
- sensation of current flowing along arms when trying to bend the neck.
Syndromes
Symptoms of cervical osteochondrosis are not considered typical. Which of them are most pronounced depends largely on the specific target. Many of the manifestations can be mistakenly associated with other pathological conditions. Therefore, there are often cases when the wrong treatment is prescribed.
The complex of symptoms is divided into the following groups:
- radicular;
- vertebral artery syndrome;
- irritative-reflex syndrome.
Radicular Syndrome
Its second name is cervical sciatica. The syndrome develops as a result of pinching of the nerve endings in the neck. The pains are transmitted down from the neck, given to the shoulder blades, down along the shoulder along the outside of the forearm to the fingers. In this case, often appear:
- creepy feeling;
- tingling of the hand, forearm, fingers;
- pasty.
Manifestations also vary depending on the area of the lesion. If the endings of the central nerve are affected, the pastiness extends to the thumb, middle, index fingers. When the endings of the brachial nerve are pinched, the little finger and ring finger are affected.
Irritative-reflex syndrome
Burning sharp pain in the cervico-occipital region, appearing during movement after a static state: after sleep, when sneezing, a sharp turn of the head, becomes its sign. Often the pain radiates to the shoulder and chest.
Vertebral Artery Syndrome
Symptoms of cervical osteochondrosis are:
- throbbing or burning headache (paroxysmal or persistent), spreading to the temporal region, the crown of the head, the back of the head, and the brow ridges;
- increased discomfort with certain movements or after a long stay in an uncomfortable position;
- general weakness;
- nausea;
- loss of consciousness;
- hearing problems;
- disorders of the vestibular apparatus;
- eye pain;
- blurred vision.
Cardiac syndrome
With the appearance of this complex of symptoms of osteochondrosis of the neck, an almost similar picture of angina develops, which often leads to erroneous treatment.
Muscle contractions and spasms in the region of the heart are most likely a reflex response to compression of the nerve endings in the lower cervical region. Cardiac syndrome is a consequence of irritation of the phrenic nerve (its fibers lead to the pericardium) or the pectoralis major muscle:
- pains appear suddenly, last a long time;
- aggravated by a sharp movement of the neck, coughing, sneezing;
- tachycardia and extrasystole are possible;
- the pain does not stop after taking coronary enlargement drugs;
- there are no signs of impaired circulation on the ECG.
Exacerbation of the disease
At the stage of exacerbation, the symptoms of cervical osteochondrosis are:
- increased pain and its irradiation to the scapula, interscapular zone, arms, shoulders;
- Difficulty in the movement of the shoulders, torso, arms, sometimes breathing (inhalation and exhalation);
- pain syndrome often resembles a heart attack or intercostal neuralgia;
- when pain appears in the right hypochondrium or iliac area, the clinic is similar to the manifestations of gastritis or cholecystitis;
- headaches are of a prolonged nature, imbalance, visual and auditory functions are disturbed;
- in the innervation zone, the trophicity of the skin is disturbed, tingling, numbness, dryness, pallor, burning, chilliness appear;
- the tone of the cervical muscles increases;
- weakness, lethargy, nervous tension, anxiety, emotional instability appear;
- possible sleep disturbances, memory disturbances, and problems with concentration.
Osteochondrosis and vegetative-vascular dystonia
Cervical osteochondrosis can lead to subluxation of the first cervical vertebra with displacement to the right or left, which provokes the development of VSD (vegetative vascular dystonia). It is quite difficult to identify it, since often there are no symptoms or they are mild. In this case, it is possible:
- compression of the sympathetic nerve plexuses, leading to the appearance of neurological signs or VSD;
- compression of arteries and impairment of cerebral circulation;
- compression of veins, provoking a violation of blood outflow and a subsequent jump in intracranial pressure;
- compression of the spinal cord, provoking a deterioration in the movement of the cerebrospinal fluid, which also results in high pressure inside the skull;
- muscle spasm that aggravates symptoms as a result of severe compression of blood vessels and nerves.
The resulting processes are:
- headaches;
- darkening in the eyes;
- dizziness;
- impaired visual acuity;
- double vision (diplopia);
- flashing before the eyes of "flies";
- high or low pressure;
- nausea, sometimes with vomiting;
- loss of consciousness.
Vertebral subluxation is detected by x-ray. Its reduction is a rather complicated procedure, usually performed under general anesthesia.
How the disease is diagnosed
The leading methods of diagnosing cervical osteochondrosis are:
- radiography;
- magnetic resonance imaging;
- computed tomography;
- Doppler ultrasound;
- duplex scanning.
The last two methods are used to check the condition of the neck vessels.



































